Signed in as:
filler@godaddy.com
Signed in as:
filler@godaddy.com
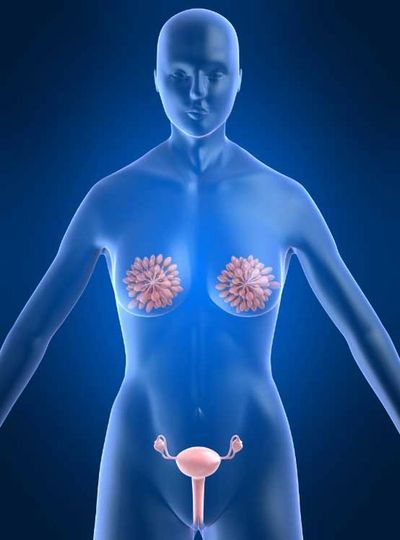
Beta hCG hormone; The human chorionic gonadotropin (hCG) test is done to check for the hormone hCG in blood or urine. HCG is made by the placenta during pregnancy. HCG may also be made by certain tumors, especially those that come from an egg or sperm. (These are called germ cell tumors.) HCG levels are often tested in a woman who may have abnormal tissue growing in her uterus. The test also may be done to look for molar pregnancy or a cancer inside the uterus. Several hCG tests may be done after a miscarriage to be sure a molar pregnancy is not present. In a man, hCG levels may be measured to help see if he has cancer of the testicles.
Cervicitis is an inflammation of the cervix, which can be due to irritation, infection, chemical or physical irritations, allergies or injury of cells that line the cervix. These irritated or infected tissues may become red, swollen, and ooze mucus and pus. They may also bleed easily when touched. Cervicitis is common. It may be caused by a number of factors. Determining the cause of cervicitis is important. If an infection is the problem, it can spread beyond the cervix to the uterus and fallopian tubes and into the pelvic and abdominal cavity and may cause a life-threatening infection. This may cause problems with fertility or the ability to become pregnant. It may even cause problems with your unborn baby if you are already pregnant.
Endometriosis is a condition in which tissue grows abnormally inside the uterus (endometrium) or outside it. Most often this is on the ovaries, fallopian tubes, and tissue around the uterus and ovaries; however, in rare cases it may also occur in other parts of the body. The main symptoms are pelvic pain and infertility. Nearly half of those affected have chronic pelvic pain, while in 70% pain only occurs during menstruation. Pain during sex is also common. Infertility occurs in up to half of the women affected. Less common symptoms include urinary or bowel symptoms. About 25% of women have no symptoms. Endometriosis can have both social and psychological effects. The cause is not entirely clear. Risk factors may include having a family history of the condition. The areas of endometriosis bleed each month, resulting in inflammation and scarring. The growths due to endometriosis are not cancerous. Diagnosis is usually based on symptoms in combination with medical imaging. Biopsy is the most sure method of diagnosis. Other causes of similar symptoms include pelvic inflammatory disease, irritable bowel syndrome, interstitial cystitis, and fibromyalgia.
Fallopian tube dysfunction means that the fallopian tube may be blocked or damaged, preventing the egg from moving from the ovary to the uterus to be implanted. The fallopian tubes can sometimes be repaired, but in vitro fertilization is usually recommended.
Causes of fallopian tube problems include the following:
• Pelvic infections (such as pelvic inflammatory disease)
• A chlamydial infection
• Pelvic infection caused by the misuse of an intrauterine device (which is rare)
• A ruptured appendix
• Surgery in the pelvis or lower abdomen
• A mis-located (ectopic) pregnancy in the fallopian tubes
Bacteria, such as those that can cause pelvic inflammatory disease or chlamydial infection, can enter the vagina during sexual intercourse with a partner who has a sexually transmitted disease. The bacteria can spread from the vagina to infect the cervix. They may then spread upward, to the uterus and sometimes the fallopian tubes. Chlamydiae can infect the fallopian tubes without causing any symptoms. These infections may permanently damage the fallopian tubes, uterus, and surrounding tissue. Scar tissue may form and block the fallopian tubes.
Other causes of fallopian tube problems include abnormalities in the pelvis that block the tubes such as:
•Birth defects of the uterus and fallopian tubes
•Endometriosis
•Fibroids in the uterus
•Bands of scar tissue between adhesions in the uterus or pelvis
Fibroadenoma of breast are benign tumors characterized by an admixture of stromal and epithelial tissue. Since both fibroadenomas and breast cancer can appear as similar lumps, it is currently recommended to perform ultrasound analyses and possibly tissue sampling with subsequent histopathologic analysis in order to perform diagnosis. Unlike typical lumps from breast cancer, fibroadenomas are easy to move with clearly defined edges. There is research suggesting that fibrocystic breast disease correlates with iodine deficiency.
From Dr. Brownstein’s book, Iodine Why You Need It and Why You Can’t Live Without It: “Animal studies have shown conclusively that an iodine deficient state can alter the structure and function of the breasts. After my own research and study, I concur with several investigators that iodine deficiency is a causative factor in breast cancer and fibrocystic breast disease. I believe it is essential that women have their iodine levels tested, and if it is shown there is an iodine deficiency, iodine supplementation should be initiated. The breasts are one of the body’s main storage sites for iodine in the body. In an iodine-deficient state, the thyroid gland and the breasts will compete for what little iodine is available. Therefore, this will leave the thyroid gland and the breasts iodine depleted and can set the stage for illnesses such as goiter, hypothyroidism, autoimmune thyroid disease, breast illnesses including cancer, and cystic breast disease. In addition, other glandular tissues such as the ovaries which contain the second highest concentration of iodine in the body, will also be depleted in an iodine deficient state.”
Hyperplasia of mammary glands is the most common type of proliferative breast condition. There are two types of hyperplasia: usual hyperplasia (more common) and atypical hyperplasia (less common). In usual hyperplasia (the most common form of hyperplasia) the proliferating (dividing) cells look normal under a microscope. Women with usual hyperplasia have about twice the breast cancer risk of women without a proliferative breast condition. In atypical hyperplasia, the proliferating (dividing) cells look abnormal. Atypical hyperplasia is less common than usual hyperplasia. Women with atypical hyperplasia have about 3-5 times the breast cancer risk of women without a proliferative condition. One study found that women diagnosed with atypical hyperplasia had about a 29 percent chance of developing breast cancer within 25 years. Atypical ductal hyperplasia (ADH) is not a form of breast cancer. Rather, it is a marker for women who may have a risk factor for developing breast cancer in the future. If you have a biopsy that shows atypical ductal hyperplasia in one of your breasts, your doctor will want to follow up on your breast health regularly.
Mastitis is an infection and inflammation of the breast. It usually is found . in the fatty tissue of the breast. It causes redness, pain and swelling. As this swelling tissue pushes on the milk ducts, it may cause pain. Mastitis is usually caused by an infection with the bacteria staphylococcus aureus. These bacteria are normally present on your skin, but cause problems when they enter the body. Bacteria causing mastitis enter through a break or crack in the skin of the breast, usually on the nipple. In fact, mastitis usually occurs in women who are breastfeeding because the nipples often become dry and irritated and can become cracked during nursing. This allows the bacteria to invade breast tissue, in particular the milk ducts and milk glands. At the same time, a clogged milk duct can mimic mastitis. Mastitis in non-breastfeeding women, is more common after menopause than before. In very rare cases, this may indicate the presence of another primary disease, such as breast cancer. While a woman adjusts to breastfeeding a new infant, the milk ducts inside the breast can become clogged, causing tenderness, redness, lumps and even heat under the skin surface, but without infection.
Menopause is the permanent end of the menstruation cycles. It is not a disease, but it can have a big impact on a woman’s well-being. Menopause can bring physical discomfort from hot flashes, night sweats, may cause sleep issues, vaginal dryness and other symptoms. Age is the leading cause of menopause. It’s the end of a woman’s childbearing years, brought on by the ovaries gradually slowing down. Certain surgeries and medical treatment can induce menopause. Those include surgical removal of the ovaries (bilateral oophorectomy), chemotherapy, and pelvic radiation therapy. Having a hysterectomy (surgical removal of the uterus) without removing the ovaries does not lead to menopause, although you will not have periods anymore. There is no proven way to predict menopausal age. It’s only after a woman has missed her periods for 12 straight months without other obvious causes, that menopause can be confirmed.
Ovarian cysts can vary, such as dermoid cysts and endometrioma cysts. However, functional cysts are the most common type. The two types of functional cysts include follicle and corpus luteum cysts.
During a woman’s menstrual cycle, an egg grows in a sac called a follicle. This sac is located inside the ovaries. In most cases, this follicle or sac breaks open and releases an egg. But if the follicle doesn’t break open, the fluid inside the follicle can form a cyst on the ovary. Follicle sacs typically dissolve after releasing an egg. But if the sac doesn’t dissolve and the opening of the follicle seals, additional fluid can develop inside the sac and this accumulation of fluid causes a corpus luteum cyst. Other types of ovarian cysts include: dermoid cysts which are sac-like growths on the ovaries that can contain hair, fat, and other tissue. Cyst-adenomas are non-cancerous growths that can develop on the outer surface of the ovaries. Endometriomas are tissues that normally grow inside the uterus but develop outside the uterus and attach to the ovaries, resulting in a cyst. Some women develop a condition called polycystic ovary syndrome. This condition means the ovaries contain a large number of small cysts. It can cause the ovaries to enlarge, and if left untreated, polycystic ovaries can cause infertility. (see iodine, under minerals)
Often times, ovarian cysts do not cause any symptoms. However, symptoms can appear as the cyst grows. Symptoms may include:
• abdominal bloating or swelling
• painful bowel movements
• pelvic pain before or during the menstrual cycle
• painful intercourse
• pain in the lower back or thighs
• breast tenderness
• nausea and vomiting
Severe symptoms of an ovarian cyst that require immediate medical attention include:
• severe or sharp pelvic pain • fever • faintness or dizziness • rapid breathing
These symptoms can indicate a ruptured cyst or an ovarian torsion. Both complications can have serious consequences if not treated early.
Ovulation was commonly believed to occur whenever we were having regular menstrual flow with normal-length menstrual cycles of 21-35 days apart. The Centre for Menstrual Cycle and Ovulation Research or CeMCOR and other groups of scientists, now show that variability in ovulation and huge variations in the amount of progesterone that each menstrual cycle makes, are very common. This frequent but not obvious cycle variation is called an “ovulatory disturbance” that includes not releasing an egg (anovulation) as well as releasing an egg with too short a time from egg-release to the next flow (short luteal phase). Ovulatory disturbances are silent within regular and normal menstrual cycles. It is still true, however, that irregular or far apart cycles are even more likely to have ovulatory disturbances. Who’s at increased risk for silent, ovulatory disturbances? We don’t know for sure because few studies have tracked women’s cycles for ovulation over extended periods. Adolescent and young women (in the first 10 years after first period or menarche) are more likely to have ovulatory disturbances. Irregular flow is also common in the first year.
Women in perimenopause have increasing ovulatory disturbances. Luteal lengths can be normal but progesterone production may be too low during this life phase. Obesity is associated with ovulatory disturbances. Cigarette smoking may also be associated with ovulatory disturbances. Although the most common reason for having a regular cycle with too little or no progesterone production is being under stress. The perceived “threat” can be physical (illness, over exertion), emotional (break-up with a partner, grief, depression), nutritional (not being able to afford or get to, enough nutritious food or not eating enough for the body’s needs), social (bullying, sexual abuse, social isolation) or spiritual (not feeling life has fundamental meaning). Thus CeMCOR investigators have come to see a normally ovulatory, regular menstrual cycle as a sign of health and well-being.
Pelvic Inflammatory Disease or PID, is an infection of the organs of a women’s reproductive system. It includes the uterus, ovaries, fallopian tubes, and cervix. It’s usually caused by a sexually transmitted infection (STI), like chlamydia or gonorrhea, and is treated with antibiotics.
You might not notice any symptoms of PID early on but as the infection gets worse, you can experience; • pain in your lower belly and pelvis • heavy discharge from your vagina with an unpleasant odor • bleeding between periods • pain during sex • fever and chills • pain when you pee or a hard time going
PID can cause serious problems if it’s not treated. For example, you might have trouble getting pregnant or have pain in your pelvic area that doesn’t go away.
Premenstrual Syndrome (PMS); Premenstrual syndrome (PMS) is a combination of emotional, physical, psychological, mood disturbance that occurs after a woman’s ovulation. Typically it ends with the onset of her menstrual flow. The most common mood-related symptoms are irritability, depression, crying, oversensitivity, and mood swings. The most common physical symptoms are fatigue, bloating, breast tenderness (mastalgia), acne, and appetite changes with food cravings. A more severe form of PMS, known as premenstrual dysphoric disorder (PMDD), also known as late luteal phase dysphoric disorder, occurs in a smaller number of women and leads to significant loss of function because of unusually severe symptoms. The American Psychiatric Association characterizes PMDD as a severe form of PMS in which anger, irritability, anxiety or tension are especially prominent. About 90% of women experience premenstrual symptoms at some point in their lifetime. The true incidence of PMS has often been overestimated by including all women who experience any physical or emotional symptoms prior to menstruation. It is estimated that clinically significant PMS (which is moderate to severe in intensity and affects a woman’s functioning) occurs in 20% to 30% of women. It is generally most severe in women in their 4th decade of life
Vaginitis is inflammation of the vagina. In premenopausal women, infection is the most common cause. After menopause, a low level of estrogen often leads to vaginal atrophy (atrophic vaginitis). Vaginitis also can be the result of an allergic reaction to an irritating chemical, such as a spermicide, douche or bath soap. Almost all infectious vaginitis is caused by one of three infections. Bacterial vaginosis is a change in the type of bacteria that normally live in the vagina, and it is the most common cause of an abnormal vaginal discharge or an unpleasant vaginal odor. In bacterial vaginosis, normal lactobacillus bacteria are replaced by other bacteria. This includes prevotella, mobiluncus, G. vaginalis, and mycoplasma hominis. The exact reason for this change is unknown. In pregnant women, bacterial vaginosis can increase the risk of a premature delivery. Candida vaginal infections, also called vaginal yeast infections, typically are caused by the Candida albicans fungus. During a lifetime, 75% of all women are likely to have at least 1 candida vaginal infection, and up to 45% have 2 or more. Women tend to be more susceptible to vaginal yeast infections if their bodies are under stress from poor diet, lack of sleep or illness, if they are pregnant, taking antibiotics/birth control pills or douching too often. Women with diabetes or human immunodeficiency virus (HIV) are more likely to have recurrent yeast infections. Trichomonas vaginitis, also called trichomoniasis, is a sexually transmitted disease (STD) caused by a microscopic one-celled organism called trichomonas vaginalis. Trichomonas causes inflammation of the vagina, cervix and urethra in women. In pregnant women, Trichomonas infections also can increase the risk of premature rupture of the membranes and preterm delivery.
Symptoms Bacterial vaginosis causes an abnormal grayish-white vaginal discharge with a foul-smelling vaginal odor. Candida vaginitis can cause the following symptoms: • vaginal itch or soreness • a thick yogurt-like vaginal discharge • burning discomfort around the vaginal opening, especially if urine touches the area • pain or discomfort during sexual intercourse
Trichomonas organisms can live in the vagina for many years without causing any symptoms. If symptoms occur, they can include: • a yellow-green, foul-smelling vaginal discharge • vaginal pain or itching • irritation and inflammation around the vaginal opening • discomfort in the lower abdomen • vaginal pain during sexual intercourse • burning discomfort during urination Symptoms may worsen during a menstrual period
Copyright © 2019 Coconutz Health - All Rights Reserved.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.